Journal of Advances in Medicine and Medical Research
Volume 35, Issue 22, Page 54-61, 2023; Article no.JAMMR.106967 ISSN: 2456-8899
(Past name: British Journal of Medicine and Medical Research, Past ISSN: 2231-0614, NLM ID: 101570965)

Improved Range of Motion and Decreased Complications After Total Knee Arthroplasty with Use of Plethy Recupe Remote Patient Monitoring: A Retrospective Study
Timothy Hui a*, Hunter Greene b, Paul Sasaura b, Subu Subramanian a, Bereket Ayalneh Sharew a and Yordanos Woldebirhan a
a Plethy Inc., San Jose, CA, USA.
b Summit Orthopedics, Carmichael, CA, USA.
Authors’ contributions
This work was carried out in collaboration among all authors. Author TH created the framework for the data analysis and clinical significance and was the primary author of the text. Authors BAS and YW performed data analysis and presentation of the results of this study. Author SS reviewed and verified the data and text. Authors HG and PS added guidance to the analysis of the data.
All authors read and approved the final manuscript.
Article Information
DOI: 10.9734/JAMMR/2023/v35i225246
Open Peer Review History:
This journal follows the Advanced Open Peer Review policy. Identity of the Reviewers, Editor(s) and additional Reviewers, peer review comments, different versions of the manuscript, comments of the editors, etc are available here:
https://www.sdiarticle5.com/review-history/106967
Received: 28/07/2023
Accepted: 04/10/2023
Published: 10/10/2023
ABSTRACT
Background: Home exercise plans (HEP) are key to recovery from surgeries, but poor compliance limits benefits. Digital health shows promise in improving compliance. This retrospective study compared pain, range of motion (ROM), and manipulation under anesthesia (MUA) complications after a total knee arthroplasty (TKA) from one clinic where one group used digital health and another did not.
Methods: Patient population was all TKA patients from 9/1/21 to 4/30/22. For rehabilitation, 41 patients used Recupe, a digital app that instructs and monitors home exercises along with live coaching. 95 patients did not. Age, gender, and BMI between both groups were very similar.
Results: ROM improved significantly with the use of Recupe, improving to 120 degrees after 1 month – a key ROM for function. The non-Recupe group improved to 112 degrees in the same timeframe.
The need for MUA was significantly better for the Recupe group, where 2% required MUA versus 5% for the other group, indicating a lower risk of major complications.
Pain averaged 2.34/10 for the Recupe group after 1 month versus 2.86/10 for the non-Recupe group, though not statistically significant.
The Recupe group performed their exercises an average of 5.1 times per week.
Conclusions: The Recupe group and the Non-Recupe group both attended medical and physical therapy visits, so the significant differences in results are likely due to non-adherence of HEP by the Non-Recupe group. This suggests that lengthened musculoskeletal recovery amongst workers may be due to non-adherence to prescribed care plans, and that digital health may improve their compliance.
Use of Recupe during rehabilitation after a Total Knee Arthroplasty results in significantly faster ROM improvement and significantly decreased risk of Manipulation Under Anesthesia. Pain was also decreased though not to statistical significance.
1. INTRODUCTION
Home exercise plans (HEP) are commonly prescribed after orthopedic injuries or surgeries. Studies have shown that these HEPs are important for full recovery and improved outcomes in various procedures [1,2]. However, in practice, poor HEP adherence has been shown to be common [3]. In current practice, providers merely ask patients what exercises have been performed, which has been shown to be overestimated in diaries and with less than acceptable reliability [4]. Even with regular physical rehabilitation visits to see a therapist, most of the rehabilitative program time is at- home, where non-adherence to prescribed at- home rehab exercises has been estimated to be as high as 70 % [5].
Successful postoperative rehabilitation has been shown to lead to shorter hospital stays, fewer complications, reduced utilization of follow-up services, and improved patient pain, activity, and quality of life outcomes [6,7]. Furthermore, home exercise plans performed prior to surgery, known as pre-habilitation exercises, have also been demonstrated to improve post-operative outcomes [8,9], reduce length of hospital stay [10], and even reduce pre-operative patient anxiety [11]. More specifically, evidence supports improved immediate recovery after procedures such as Total Knee Arthroplasty (TKA) [12,13].
Previous studies have shown progress after TKA and benefits from rehabilitation. A study [14] showed an average increase in ROM of 27% after two weeks and 50% after 6 weeks. Another study showed similar results with knee flexion ROM utilizing home exercises without direct supervision compared to in person physical therapy [15].
In terms of pain, researchers tracked patient’s recovery after Total Knee Arthroplasty (TKA) in a study performed at Northwestern University [16]. These patients received both inpatient (hospitalization) and outpatient physical therapy, and after one month, they reported an average pain of 3.68 when set on a 1-10 scale, with 44% of patients demonstrating a pain level of 4/10 or greater.
Complications can be a major problem after surgery and a cause for increased medical use and cost. Infections can result in further surgeries and a poor outcome [17]. Another common complication after joint replacement surgery is the failure to regain an adequate range of motion. In these cases, a manipulation under anesthesia (MUA) is a common treatment [18], with a frequency between 0.5 and 10% [19]. Aside from being another procedure, MUA after TKA is associated with worse outcomes, including an increased chance for future revision surgeries [20]
For post-surgical recovery, measured by ROM, pain, and complications, it is possible that improved HEP adherence could result in improved outcomes. However, previous methods of tracking these have had challenges [4,5].
One method to measure and ensure exercise adherence outside of medical offices is through digital health with wearable tracking sensors. Plethy offers this solution through their Recupe app and sensor. Working with healthcare providers, Recupe can give patients physician directed, remote supervised rehabilitation. Patients and clinicians receive objective, real- time feedback on performance, and have a record of the data from their home exercise sessions. This holds patients accountable to their healthcare provider for rehab performed without in-person supervision.
Along with adherence, Recupe tracks pain, joint range of motion with exercises, red flag symptoms, patient engagement, and patient behavioral/sentiment. Pain and sentiment correlations have been shown [21]. ROM accuracy was researched and found to be over 90% accurate [22]. Recupe supports surgical and non-surgical diagnoses, exercises throughout the treatment plan including pre- surgical, enables remote monitoring, and provides visibility to physical training sessions and care journey data. Alerts for red flag symptoms and surgery site pictures are also part of the direct communication with doctors provided by Recupe.
In this study, we compared outcomes after Total Knee Arthroplasty from one orthopedic practice. One group of these patients used the Recupe platform, created by Plethy. The second group did not use Recupe. We compared the pain, range of motion, and the propensity for MUA between the Recupe group and the non-Recupe Group to see if the use of Recupe would result in a significant difference in outcomes.
2. METHODS AND PROCEDURES
2.1 Subject Selection
Chart review was performed on the EHR of Summit Orthopedics in California. The cohort was identified by reviewing all patients who had a TKA performed by searching for the CPT code for TKA. 170 patients were identified. The date range of this search was from 9/1/21 to 4/30/22.
For patients using Recupe, patient engagement data was gathered from the Recupe database on these patients. The minimum use of Recupe was selected as three times per week for this study.
Three patients had TKAs on both knees. Each surgery was classified as a separate patient for this study. One patient had no data available and was removed. 13 subjects were eliminated due only performing Recupe prior to surgery. Finally, 20 subjects were eliminated because they used Recupe less than 3x per week.
The remaining patients were classified into two groups as follows:
41 patients in the Recupe group. Recupe use was on average 5.1 times per week (SD 1.21).
95 patients in the non-Recupe group.
2.2 Intervention
Patients in the Recupe group were trained in the use of the Recupe app and received weekly follow up and encouragement from coaches. Home exercise programs (HEP) were designed by doctors or physical therapists while coaches encouraged patients to adhere to their HEP.
Both the Recupe and Non-Recupe groups were prescribed outpatient physical therapy. However, our data did not give sufficient detail as to the frequency and use of these treatments
3. RESULTS
3.1 Demographics
For the Recupe group, the average age of patients was 68.11 (sd 8.87).
By gender, there were 57.14% male and 42.8% female.
Average BMI: 31.8
For the non-Recupe group, the average age was 69.35 (sd 9.44)
By gender, there were 58.95% male and 41.05% female.
Average BMI: 31.9
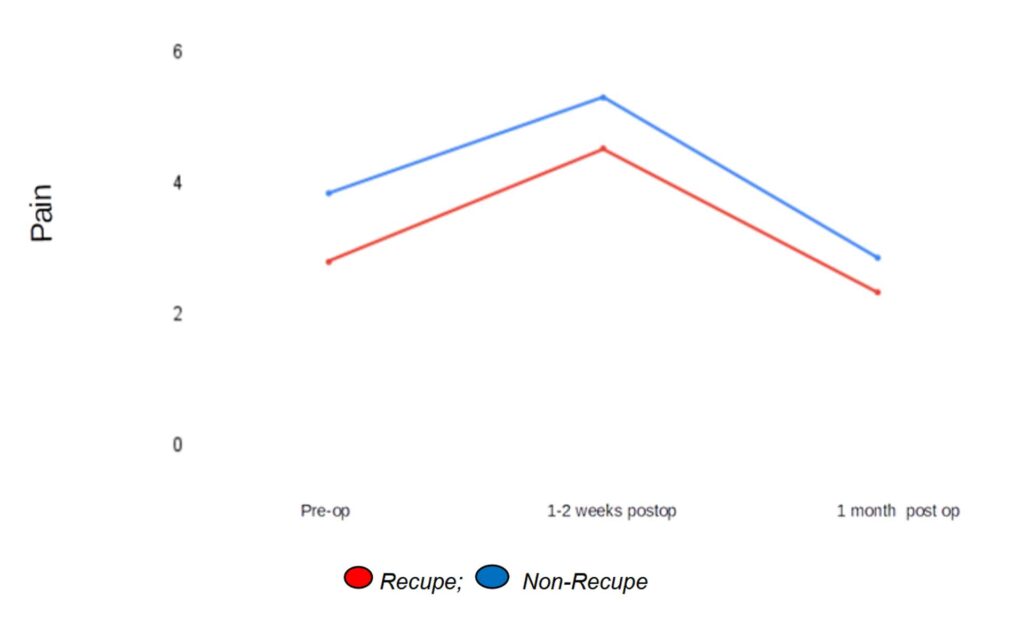
3.2 Pain
3.2.1 Post-op pain
3.2.1.1 1-2 Weeks after surgery
Pain is highest at the first visit, which occurs 1-2 weeks after surgery.
For patients using Recupe – average 4.53/10 (sd 2.55)
For all non-Recupe patients – average 5.31/10 – (sd 2.88)
p-value – .14
3.2.1.2 One month after surgery
Post-op pain decreases 1 month after surgery
For patients using Recupe – average 2.34/10 (sd 1.89)
For all non-Recupe patients – average 2.86/10 (sd 2.52)
p-value – .24
3.2.1.3 Pre-op pain
Pre-op pain was lower for Recupe patients
For patients using Recupe – average 2.80/10 (sd 2.37)
For all Non-Recupe patients – average 3.85/10 (sd 3.11)
p-value – .056
At all times, Recupe patients reported lower pain than non-recupe patients (Fig. 1).
For the Recupe group, this data came from 36 Recupe patients who did pre-op exercises, averaging 28.9 days of pre-op exercises, similar to the 4 weeks to 8 weeks often used for pre- operative studies [21].
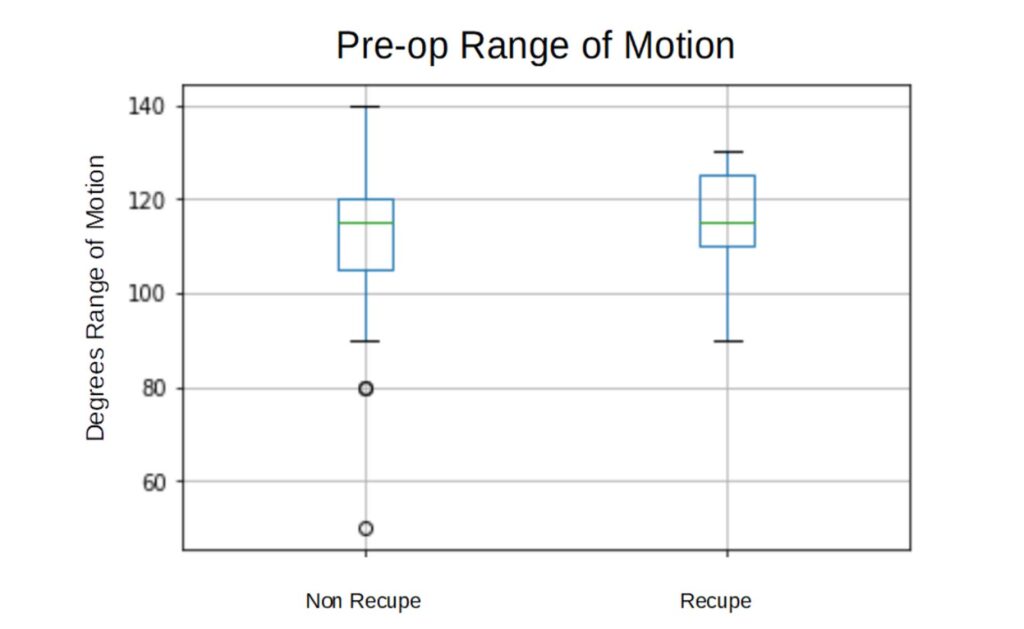
3.3 Range Of Motion (ROM)
3.3.1 Pre-op knee flexion ROM
Recupe – average 114 degrees (sd 10.76) Non recupe – average 112 degrees (sd 13.69)
p-value – .18
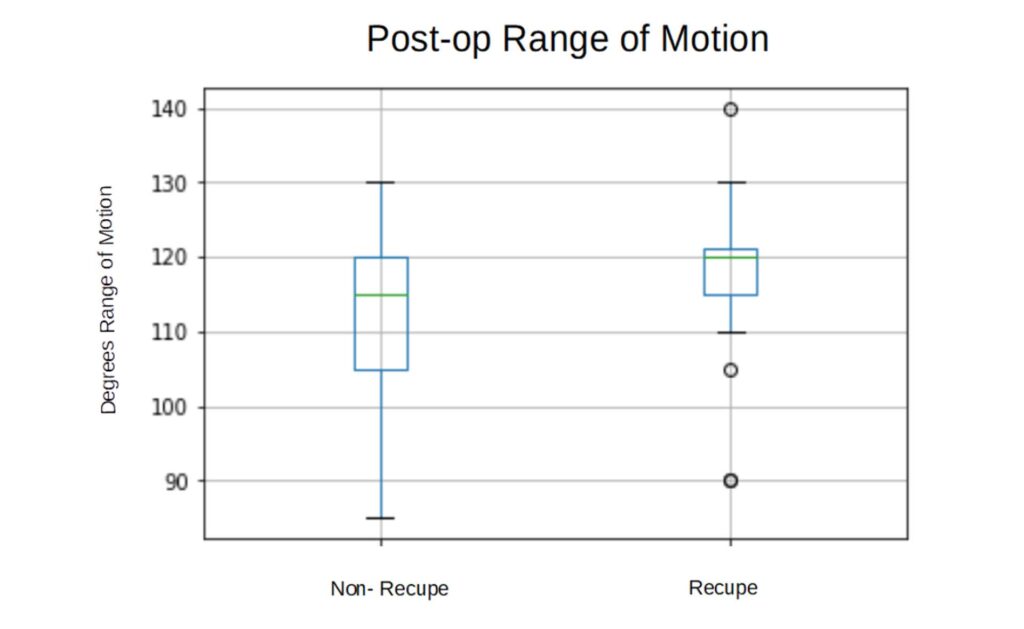
3.3.2 1 Month Post op knee flexion ROM
For patients using Recupe – average 120 degrees (sd 9.08)
For all Non-Recupe patients – average 112 degrees (sd 11.56)
p-value – .0037
Knee flexion ROM starts with no significant difference between groups, but after surgery, Recupe patients have significantly improved knee flexion ROM (Fig. 2 and Fig. 3). Also, there is less variation between patient’s ROM for those using Recupe, and hence fewer negative outliers. This data excludes 1-2 week post-op ROM data
due to this data being missing in a large portion of patients.
3.4 Complication – Manipulation under Anesthesia
Manipulation under anesthesia was significantly less likely for patients who used Recupe 3x per week.
non-recupe – 111 patients – 5 MUA – 5%
Recupe – 41 patients – 1 MUA – 2%
P-value – less that 1.0 e-25.
So, Recupe patients had a significantly reduced risk of MUA.
4. DISCUSSION AND CONCLUSION
For this study, three times a week was chosen as the exercise frequency for inclusion due to support from research [23]. With this frequency, use of Recupe appears to provide an advantage in pain, ROM, and complications.
Demographically, the population of both groups was very similar, and at ages where tech familiarity can be poor. Still, with an average of 5.1 sessions per week, adherence was excellent.
In terms of pain, while the p-value was not as strong, the pain reported was lower for those who used Recupe. The closest to the desired alpha level of .05 was for pre-op pain, where the patients performed close to the minimum range of 30 days of pre-op exercises used in prior research [24], so it is possible that a longer pre- operative program could have resulted in more significant values. Compared to the study cited earlier [16], both groups demonstrated lower pain after one month. With lower pain reported compared to previous research, there also appears to be no decrease in quality from exercise without in-person supervision [15].
For Range of Motion, the Recupe group demonstrated greater ROM, indicating improved recovery, and the average reached 120 degrees, which is often used as a target for recovery [25]. Per a previous study on TKA ROM progression, the non-Recupe group would take 25 days to reach 120 degrees [26]. From the same study, the Recupe group’s ROM is around the 85th percentile. Also with less variation in results, there were fewer outliers in the Recupe group. So, most of this group would have a functional ROM and hence there are fewer outliers with inadequate ROM.
This leads directly to the lower percentage of MUA for Recupe patients. Since MUA is performed on patients who are failing to recover their knee ROM, the fewer negative outliers for the Recupe group result in fewer MUA. This is very significant due to the potential complications from additional procedures, as well as the costs to patients and the medical system. Also, MUAs are associated with many poor outcomes, including a knee revision [20], and increased societal cost such as prolonged recovery and more healthcare utilization.
Overall, these results show advantages over the non-Recupe group. It is important to note that many in the non-Recupe group attended outpatient physical therapy and all were given some home exercises. Some in the Recupe group also attended physical therapy. The use of outpatient physical therapy could affect the outcomes such as pain and ROM. Unfortunately, the records did not contain sufficient data on physical therapy used. What can be confirmed is that the Recupe group performed exercises at least 3 times per week, with an average of 5.1 days per week. This is substantially better than the up to 70% non-adherence from previous studies [5].
With the benefits shown in the Recupe group, it appears that this form of physician directed remote supervision provides benefits without in- person physical therapy, as previous research showed [15], and could be superior to physical therapy alone, likely due to increased engagement [5]. This suggests that improved adherence to home exercises plans may be an important facet to speeding recovery and reduction of cost, be it in orthopedic group health or other arenas such as worker’s compensation.
There were some limitations to this study. First, though the demographics were very similar, the populations were not randomized. Second, there were gaps where data was not recorded, such as knee flexion ROM 1-2 weeks after surgery. Also, physical therapy and exercises performed outside of Recupe were not recorded or controlled. Finally, multiple patients started Recupe, but either did not use it often enough, or did not use it after surgery.
5. FUTURE RESEARCH POSSIBILITIES
Statistical analysis will reveal relationships between all these variables. In addition, predictive analytics is expected to deliver recovery maps, personalized care plans, and continuous risk stratification. Insights delivered from analytics are expected to significantly enhance the Recupe solution by enabling identification of non-adherent patients and by understanding what patient-specific variables are most likely to improve pain and function outcomes.
While this data shows a significant reduction in MUA with use of Recupe, further research is required in this area. A greater number of MUAs from a larger population could better demonstrate the relationship between Recupe and MUAs after TKA.
DISCLAIMER
This paper is an extended version of a preprint document of the same author.
The preprint document is available in this link:
https://www.researchsquare.com/article/rs- 2697935/v1
[As per journal policy, preprint article can be published as a journal article, provided it is not published in any other journal].
CONSENT AND ETHICAL APPROVAL
Study IRB approval and Conflict of Interest review have been completed through the institutional review board (IRB) of the Biomedical Research Alliance of New York (BRANY). All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by BRANY. The need for informed consent was waived by the IRB/Ethics committee of BRANY.
COMPETING INTERESTS
Authors have declared that no competing interests exist.